Peripheral Vascular Disease – A Stealthy Disease Not to Be Ignored
What is Peripheral Vascular Disease?
Peripheral Vascular disease is a blood circulation disorder that causes restricts blood flow to parts of the body other than the brain and heart. PVD is a circulatory problem in which narrow arteries reduce the blood flow to the limbs. This disorder causes the blood vessels (arteries (or) veins) located outside of the heart and brain to narrow, block or spasm.
This means that when peripheral vascular disease part of your body outside the heart and the brain does not receive enough blood flow to keep with demand. When narrowing occurs in the heart called coronary artery disease.
Peripheral Vascular disease most commonly affects the legs but can also affect the blood vessels that supply blood and oxygen to the arms, stomach, and kidneys. People over the age of 50 are believed to suffer more from peripheral vascular disease and it is slightly more common in men than in women.
Types of Peripheral Vascular Disease
The Two main types of peripheral vascular disease are:
- Organic PVD
- Functional PVD
Organic PVD: Organic PVD results from structural changes in blood vessels caused by inflammation, plaque build-up, tissue damage.
Functional PVD: Functional PVD results as a result of decreased blood flow in response to something that triggers the blood vessels to either narrow or changes in body Temperature.
Causes for Peripheral Vascular Disease:
Organic Peripheral Vascular Disease is usually caused by atherosclerosis – a condition in which plaque build up in the blood vessels. Common risk factors of atherosclerosis include:
- Smoking
- High Blood Pressure
- Diabetes
- High Cholesterol
- Arthritis, lumps
- Insulin Resistance
- Blood clots
Other conditions that may cause structural changes in blood vessels are Deep vein thrombosis (DVT), varicose veins, chronic venous insufficiency and Reynaud’s syndrome.
Functional PVD is caused by
- Cold Temperature
- Drug use
- stress
- Obesity
What are the Risk Factors for Peripheral Vascular Disease?
There are a number of risk factors for peripheral vascular Disease
- Being over the age of 50
- A family history of stroke or PVD
- High levels of homosysteine
- Over weight
- History of Coronary Or Cerebrovascular Disease
- Kidney disease on hemodialysis
Symptoms for Peripheral Vascular Disease:
Just around 60% of people with peripheral vascular disease have symptoms. Quite often, symptoms are caused by the leg muscles not getting sufficient blood. Other symptoms of PVD is include
- Painful Cramping in hip & thighs
- Leg numbness or weakness
- Coldness in leg
- Sores on feat that won’t heal
- Change in the colour of leg
- Weak Pulse
- Erectile dysfunction in men
- Shiny legs
- Claudication
- Gangrene
- Ulcers On Your Toes
Diagnosis of peripheral vascular disease:
After reviewing your family and medical history which includes details of lifestyle, diet and medication use, A Interventional Radiologist performs a physical examination which includes checking skin temperature appearance and the presence of a pulse in the leg and feet.
Further testing of PVD may include:
- Ankle-Brachial Pressure Index (ABPI)
- Doppler Ultra sound scan
- Magnetic Resonance Angiography (MRA)
- Computerized tomography angiography (CTA)
- Catheter Angiography
ABPI estimation and Doppler scan are the most usually utilized modalities to diagnose peripheral vascular disease. CTA/MRA is utilized when revascularization is planned.
Must Read: What Are Uterine Fibroids and what is the best treatment?
Treatments for PVD:
Effective PVD treatment aims to slow or stop disease progression, manage pain and other symptoms, and diminish the risk of serious complications.
PVD treatment plans usually include the way of lifestyle changes. Some people may also require medication.
Life Style changes:
Way of life changes includes:
- Participating in standard exercise, including walking
- Eating a balanced diet
- Losing weight if necessary
- Quitting smoking
Medication:
Medications to treat PVD include:
- Cholesterol-lowering medications.
- High blood pressure medications
- Medication to control blood sugar
- Medications to prevent blood clots
- Symptom-relief medications
What are the Interventional Radiology Treatments available to treat Peripheral Vascular Disease (PVD)?
Interventional Radiology Treatments for PVD:
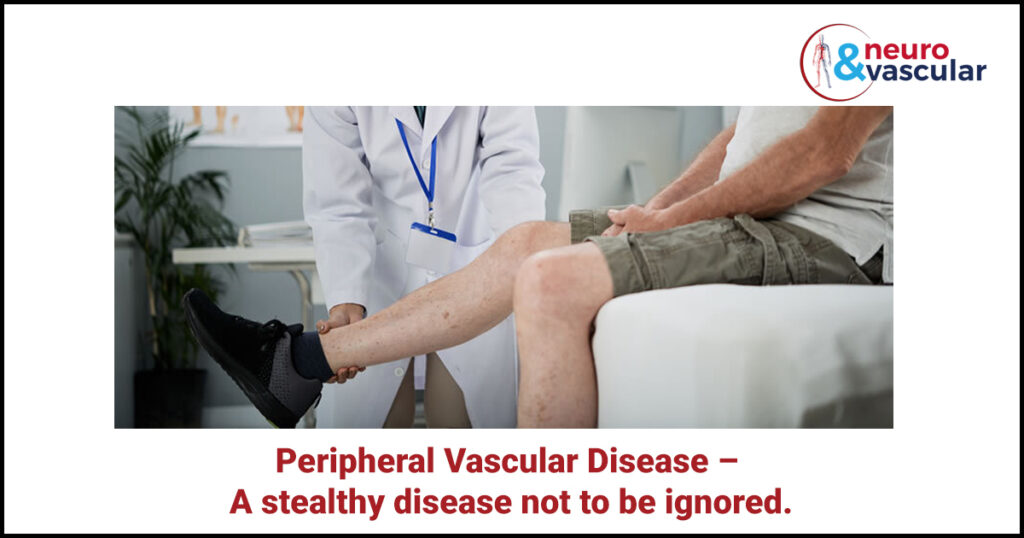
Angioplasty and Stenting:
Angioplasty is performed by An Interventional Radiologist by inserting a thin tube (catheter) into a blocked artery through a small incision. A small balloon on the tip of the catheter is expanded inside the artery to open the clog. A stent – a little wire mesh cylinder may also be put in at this time. The stent behaves like scaffolding and holds the artery open. Once in a while specialists give a medication through the catheter or then again insert a special device through it to remove a clot that’s blocking the artery.
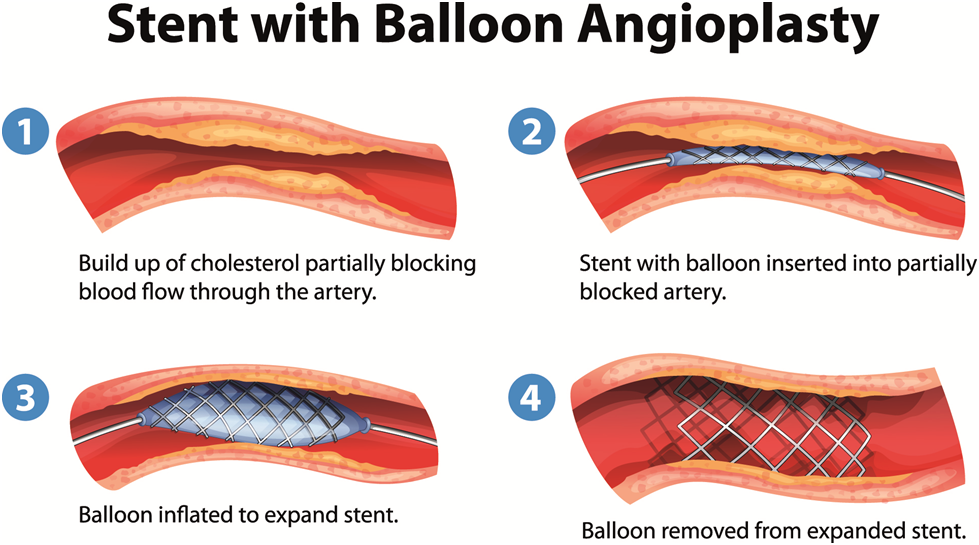
Bypass Surgery:
Surgical treatment for peripheral artery disease involves either bypass vascular surgery performed by a vascular surgeon. Indications for surgical treatment of peripheral artery disease include lesions that, for anatomical reasons, may be difficult to treat by angioplasty. Bypass surgery includes utilizing a vein from your body or a portion of synthetic vessel (known as grafts) to make a diversion around the blockage. One end of the grafts is sewn to damage the artery above the blockage and the opposite end is sewn below the blocked area. Blood circulation is then able to bypass the area of narrowing or blockage. Bypass surgery is a major surgery requiring general anesthesia and a hospital stay.
Atherectomy:
An atherectomy is a medical procedure that eliminates plaque from a blood course utilizing a catheter with a sharp edge on the end. The catheter is placed into the artery by a tiny puncture, and the procedure is done under local anesthesia. The catheter is designed to collect the removed plaque in a chamber at the tip, allowing the plaque to be removed from the artery as the device is withdrawn. The procedure can be repeated at the same time as the treatment to remove a considerable quantity of disease from the artery, thus eliminating a blockage from atherosclerotic disease.
Thrombolytic therapy:
Thrombolytic therapy involves the use of drugs known as lytics or “clot busters” to dissolve blood clots that have abruptly (suddenly) blocked your major arteries or veins and are posing a serious or life-threatening risk. The therapy must be started as soon as possible before permanent damage has occurred.
Amputation:
In severe cases of gangrene that cannot be treated, the limb may need to be surgically amputated to prevent the infection from spreading throughout the body.
Frequently Asked Questions
Q: Why does diabetes cause peripheral vascular disease?
A: The lining of your blood vessels is affected by diabetes. This indicates that your blood vessels aren’t as flexible as they should be to allow for smooth blood flow. As a result, your risk of Peripheral vascular disease increases.
Q: What are the consequences of not treating a peripheral vascular disease?
A: As plaque growth progresses, clots completely blocking the artery. If left untreated, this can result in organ damage and the loss of fingers, toes, or limbs.
Q: How is cholesterol related to peripheral vascular disease?
A: Cholesterol is a fatty substance that develops in your bloodstream. High cholesterol can hurt your arteries. That raises your risk for peripheral arterial disease (PAD) or peripheral vascular disease. This disease affects arteries in the legs.
About the Author:

Name: DR .SURESH GIRAGANI
INTERVENTIONAL RADIOLOGIST
DR. SURESH GIRAGANI CONSULTANT INTERVENTIONAL RADIOLOGIST at Yashoda group of hospitals, has more than sixteen years of clinical experience in vascular interventions with a special interest in neurovascular and peripheral vascular disease interventional procedures.