Cerebral AVM Treatments in Hyderabad
Cerebral AVMs and symptoms
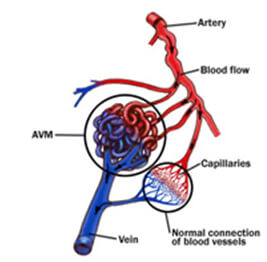
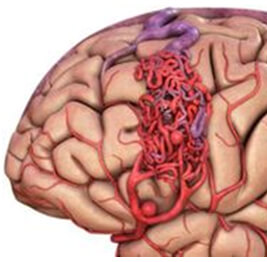
Arteriovenous malformations are masses of abnormal blood vessels that grow in the brain. They consist of a blood vessel “nidus” (nest) through which arteries connect directly to veins, instead of through the elaborate collection of very small vessels called capillaries. Some people are born with the nidus, but as the years go by, it tends to enlarge as the great pressure of the arterial vessels cannot be handled by the veins that drain it. This causes a large collection of worm-like vessels to develop (malform) into a mass capable of bleeding at some future time. These malformations are most likely to bleed between the ages of 10 – 55; after 55, the chances of bleeding diminishes rapidly. Before 55, the likelihood of hemorrhaging is betweeen 3 and 4% per year (with a death incidence of about 1%). Once an AVM patient has hemorrhaged, the risk of having another one might approach 20% during the first year, and gradually lessen to about 3 – 4% over the next few years.
AVMs can occur in any area of the brain, and may be either small or large. When they hemorrhage, they usually do so with a limited amount of blood, unlike the hypertensive hemorrhages of other stroke patients. Loss of neurologic function depends on both the location of the AVM and the amount of bleeding. Many patients have very small hemorrhages, often multiple. They may have convulsions before even knowing about the presence of an AVM. Some patients with AVMs can present with headache.
Complete Cure of a Ruptured Cerebellar AVM by Endovascular Embolisation
Cerebral AVM treatment options
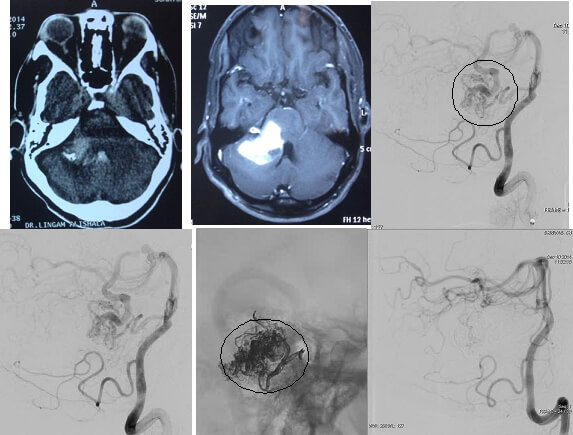
All brain AVMs presenting with bleeding should be treated. There is conflicting evidence to treat unruptured AVMs. Ruptured brain AVM can be and sometimes have to be treated by multiple modalities. Apart from surgery and stereotactic radiation therapy endovascular embolization is one of the treatment methods to obliterate ruptured brain AVMs. With the advent of newer embolic agents including Onyx, Phil, Squid, complete occlusion by embolisation is feasible especially in smaller AVMs with fewer and accessible arterial pedicles
Embolization of the AVM with liquid embolic agent (Onyx) using micro catheter to access the AVM (The right image)
The bottom image showing ruptured right cerebellar hemisphere AVM having arterial feeders from right AICA (anterior inferior cerebellar artery). Complete occlusion of the AVM achieved by endovascular onyx embolisation

Dural AVFs and symptoms
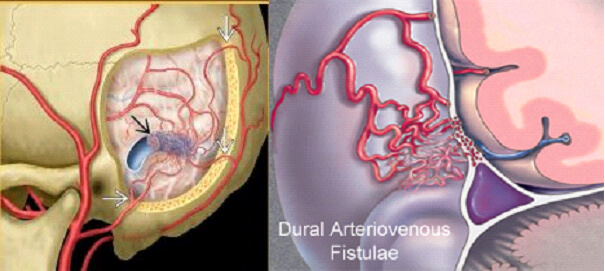
Dural Arteriovenous fistulae are abnormal communications between meningeal arteries and brain veins. These fistulae develop as a consequence of clots in the veins of the brain. Over a period, as a result of the high pressure in the brain circulation, patients tend to develop symptoms of raised brain pressure including headache and visual loss. Sometimes the veins involved in the fistulae can burst because of the pressure inside them causing brain haemorrhage. Dural AVFs are diagnosed by digital subtraction angiography
Is the Inferior Petrosal Sinus Sampling (IPSS) procedure Painful?
The Role of Interventional Radiology in the Treatment of Tinnitus
Dural AVFs treatment options
Closing of the abnormal communications between the meningeal arteries and dural veins forms the crux of the treatment. Endovascular embolisation is minimally invasive method of treatment proven to be effective in treating these lesions. Complete or near complete occlusion of these lesions will result in significant relief from the symptoms
Dr Suresh Giragani performs an embolisation procedure of first of its kind in a brain AVM patient
The carotid stenting
Stenting is a minimally invasive method for opening the blocked blood vessels by placing a stent in the artery. Carotid stenting is one of the methods to open (carotid revascularization) the blocked carotid artery (carotid stenosis). Although open surgical endarterctomy is the traditional standard for the treatment of carotid stenosis, carotid stenting of late had been proved to be not inferior to endarterectomy. Both short term and longterm results have shown no significant difference in results of stenting and endarterectomy in terms of outcomes and recurrence. (Reference – N Engl J Med 2010;363:11-23 ,’ N EnglJMed. 2016;374:1021-31).

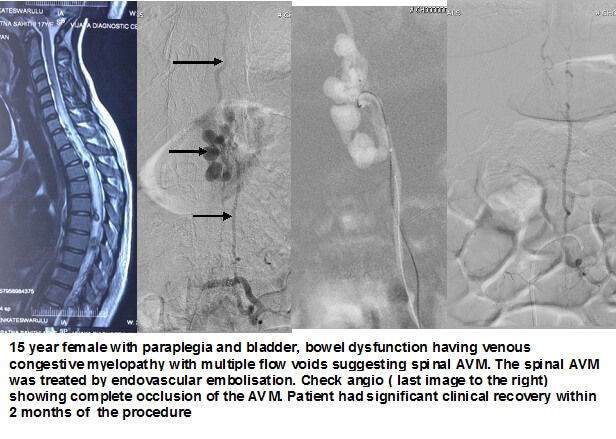
Spinal AVMs and their symptoms
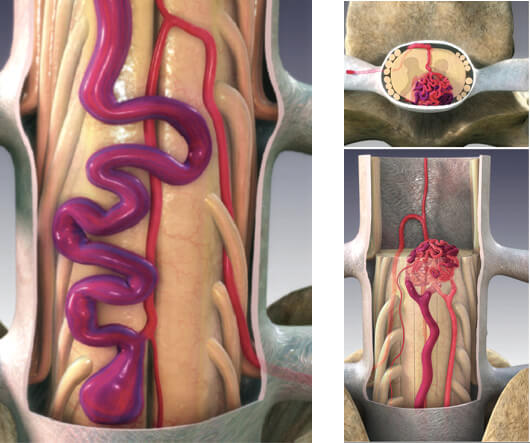
Spinal arteriovenous malformations (AVMs) are abnormal collections of blood vessels in the spinal canal that have a direct connection between the arterial system and the venous system without intervening capillaries. Eighty percent occur between ages 20 and 60. Eighty-five percent of spinal AVMs involve progressive neurological symptoms over months to years, especially back pain associated with progressive sensory loss and lower extremity weakness. Ten percent to 20 percent involve a sudden onset of weakness, numbness, difficulty urinating, urinary incontinence, fecal incontinence, or paralysis (usually in patients younger than 30) as a result of hemorrhage.
Spinal AVMs and their treatment
Magnetic resonance imaging (MRI) has increased the likelihood of identifying spinal AVM lesions. Spinal angiography is used to map the vascular structure and it is mandatory to do spinal AVM embolisation if treatment is contemplated. The treatment plan is formulated after careful consideration of the patient's clinical history, the symptoms, the physical examination and available diagnostic studies. Some of these lesions can be treated via minimally invasive endovascular embolization of the AVM to obliterate it. Lesions that have hemorrhage may additionally require surgical removal, especially those within the spinal cord or compressing the spinal cord.
DR.SURESH GIRAGANI CONSULTANT INTERVENTIONAL RADIOLOGIST at Apollo Hospital, has more than Seventeen years of clinical experience in vascular interventions with a special interest in neurovascular and peripheral vascular disease interventional procedures.
Services
Quick Links
Contact Us
Copyright 2021 Neuro All rights reserved. | Powered By KBK Business Solutions