Varicocele Embolization Treatment in Hyderabad
What is varicocele ?
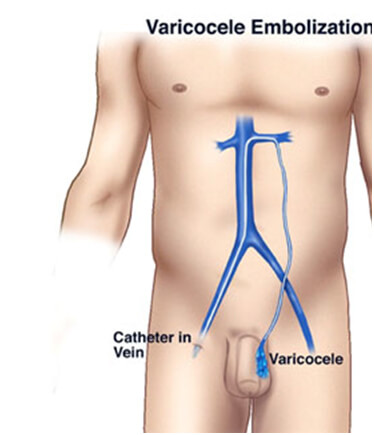
Normally, oxygenated blood flows to the testicles via an artery, and deoxygenated blood flows out via a network of small veins that drain into another vein, and is eventually carried back to the heart. During this process, backflow to the testicles is prevented by a series of one-way valves in the vein. In some individuals, however, these valves do not work well. As a result, the blood flows in reverse and causes "back pressure" to stretch and enlarge the network of small veins around the testes, forming a varicocele.
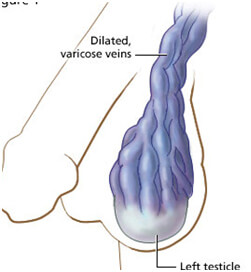
Symptoms of varicocele ?
Many times a varicocele is silent and does not cause symptoms. However, some varicoceles cause a dull or aching pain, especially when the person has been in an upright position for a long time. Heavy lifting may also cause pressure build up in the varicocele. In some individuals, a varicocele may cause decreased fertility or infertility. As many as 40% of men with decreased fertility have a varicocele. A commonly accepted theory is that the varicocele raises the testicular temperature and adversely affects the sperm count and quality. More than half of men with decreased fertility will have improvement in the sperm count and quality after treatment of the varicocele.
In some men, varicoceles can cause shrinking (atrophy) of the testicles. In many cases, when the varicocele is treated on the affected side, the testicle may return to normal size.
Varicocele is One of the Main Causes of Male Infertility You Should Know
What are the treatment options of varicocele ?
Embolization requires no stitches or general anesthesia . Nearly all the patients can be treated on an outpatient basis and may return to normal activities in two to three days. Surgical treatment requires an incision and may require several days or even weeks to return to full activities. Studies have shown that embolization and surgery are equally effective.
Advantages of Embolization
- No surgical incision in scrotal area
- As effective as surgery, as measured by improvement in semen analysis and pregnancy rates
- Patients can return to normal daily activities immediately and without hospital admittance; surgery requires several weeks’ recovery and hospital admittance
- The rare patient who has varicoceles on both sides can have them fixed simultaneously through one vein puncture site; surgery on both sides requires two separate open incisions
- No sutures
- No infections
How the procedure is done ?
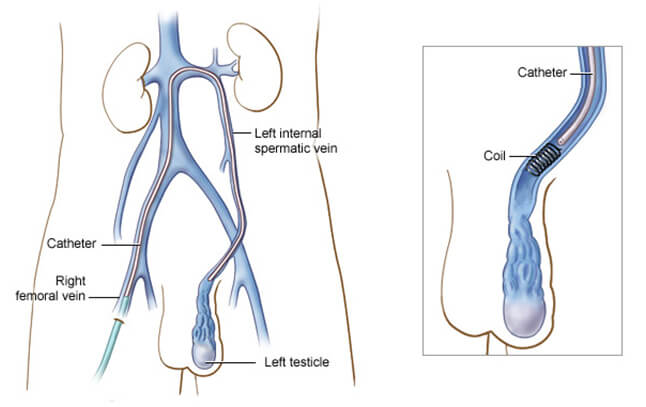
Using image-guidance, a catheter (a long, thin, hollow plastic tube) is inserted through the skin into the femoral vein, a large blood vessel in the groin, and maneuvered to the treatment site. Small amounts of x-ray dye (contrast) are injected so that the interventional radiologist can clearly see the veins on the x-ray in order to pinpoint where the problem is and where to embolize, or block, the vein. Tiny coils made of stainless steel or platinum or other materials, such as liquids, which directly close a vessel, are then inserted in the vein to block it. By blocking the diseased draining vein, backflow into the testicle is stopped and the blood is diverted to healthy veins to exit the testicle through normal pathways. Swelling and pressure within the testicle will be reduced if the blood flow is successfully diverted. At the end of the procedure, the catheter will be removed and pressure will be applied to stop any bleeding. The opening in the skin is then covered with a dressing. No sutures are needed. This procedure is usually completed within one hour
Is Endovascular Coiling The Best Treatment for Brain Aneurysms?
Success rates of embolisation
There is a 90% success rate with embolization, and of those with success, about 10% may experience late recurrence. These results are the same as those achieved with more invasive surgical techniques. Varicocele embolization has been performed for over 25 years and has an excellent long-term safety record. Its safety and effectiveness has been shown in very large trials.
DR.SURESH GIRAGANI CONSULTANT INTERVENTIONAL RADIOLOGIST at Apollo Hospital, has more than Seventeen years of clinical experience in vascular interventions with a special interest in neurovascular and peripheral vascular disease interventional procedures.
Services
Quick Links
Contact Us
Copyright 2021 Neuro All rights reserved. | Powered By KBK Business Solutions