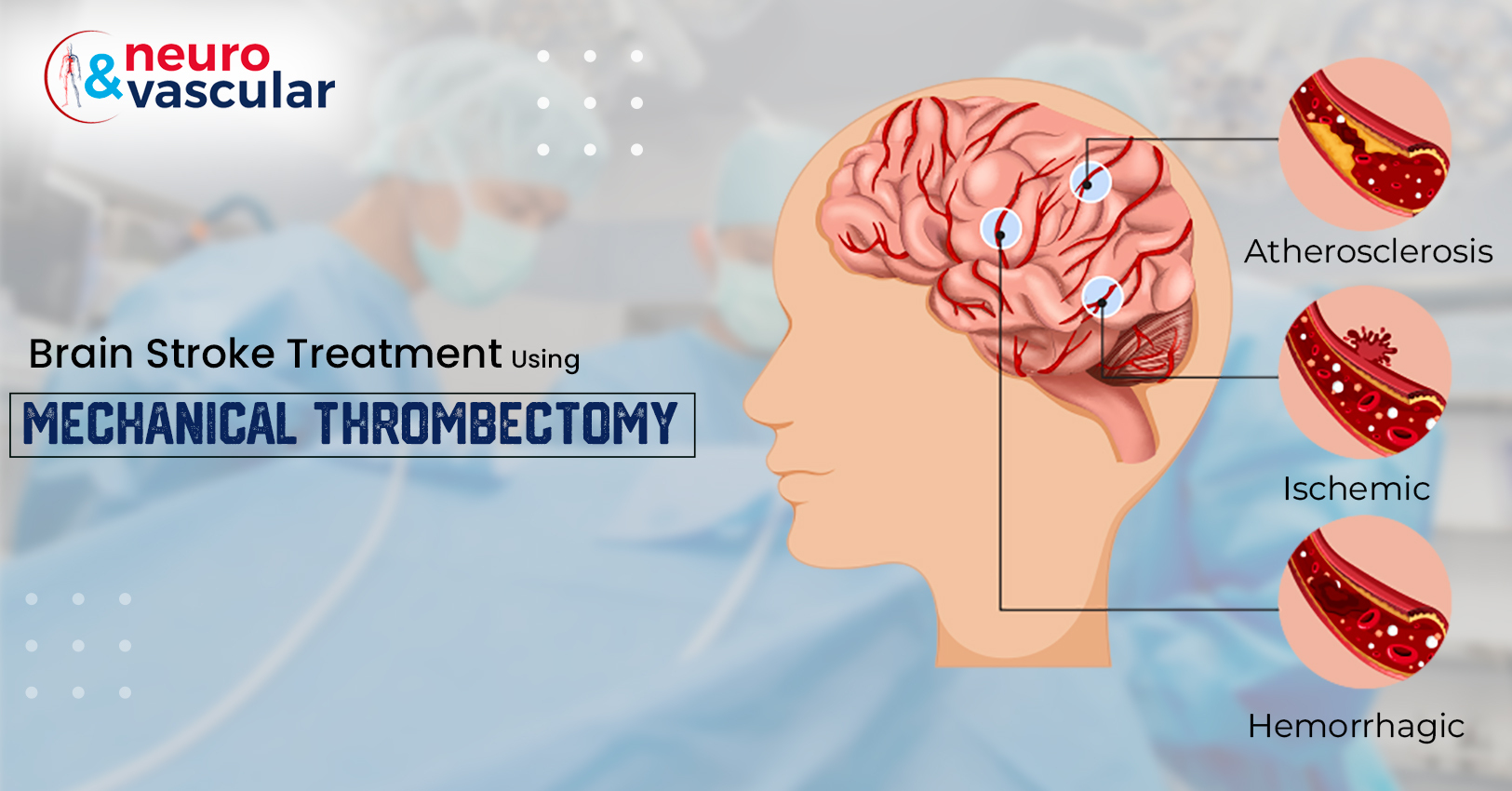
Brain Stroke Treatment using Mechanical Thrombectomy

A brain stroke, also known as a cerebrovascular accident, occurs when there is a disruption of blood flow to the brain. This can happen as a result of a blocked or ruptured blood vessel, and it can lead to damage or death of brain cells. The consequences of a brain stroke can be severe, including paralysis, difficulty speaking, and memory loss. Treatment for a brain stroke is critical and time-sensitive, as brain cells begin to die within minutes of the onset of a stroke. But one of the latest developments in stroke treatment is mechanical thrombectomy. A procedure in which doctors use a special device to remove large blood clots from an artery leading to the brain.
What is Mechanic Thrombectomy?
Mechanical thrombectomy is a minimally invasive and endovascular procedure a procedure used to remove blood clots that are blocking blood vessels in the brain. It is a treatment option for ischemic stroke, which is the most common type of stroke and occurs when a blood clot forms in an artery that supplies blood to the brain.
One of the most effective treatments for a brain stroke is mechanical thrombectomy, which is a procedure that uses a specialized device to remove the blood clot that is blocking the blood vessel. This procedure is typically performed by a neuro-interventional radiologist, a medical specialist who has been trained in the use of imaging and other technologies to diagnose and treat brain disorders.
Mechanical Thrombectomy Procedure:
The mechanical thrombectomy procedure begins with the insertion of a thin tube, called a catheter, into an artery in the groin. The catheter is then guided through the blood vessels to the site of the clot in the brain. Once the catheter is in position, a small device on the end of the catheter is used to capture and remove the clot.
The procedure typically takes between 90 minutes to 2 hours. Following the procedure, the patient is closely monitored for any complications and may need to stay in the hospital for a few days.
Mechanical thrombectomy is typically recommended for patients who have had a large vessel occlusion (LVO) stroke. A large vessel occlusion stroke is when a blood clot forms in one of the large blood vessels that supply blood to the brain, such as the middle cerebral artery. This type of stroke can cause significant damage to the brain and can be life-threatening.
Who is the candidate for Mechanical thrombectomy?
Mechanical thrombectomy for patients who have had an LVO stroke and who meet certain criteria, such as:
- Symptoms of stroke began less than 6 hours before the procedure
- Patient is able to tolerate the procedure
- Patient is a candidate for general anaesthesia
- Imaging confirms the presence of an LVO
Benefits of Mechanical Thrombectomy:
This is a procedure that uses a specialized device to remove blood clots that are blocking blood vessels in the brain. It is a highly effective treatment for large vessel occlusion (LVO) strokes, which are caused by blood clots in large blood vessels that supply blood to the brain.
The benefits are including:
- Improved outcomes: Mechanical thrombectomy has been shown to significantly improve outcomes for patients who have had an LVO stroke. It can increase the chance of survival and improve the chances of recovery.
- Faster recovery: By removing the blood clot that is blocking the blood vessel, mechanical thrombectomy can restore blood flow to the brain and prevent further damage. This can lead to a faster recovery for the patient.
- Reduced disability: By preserving brain function, mechanical thrombectomy can help to reduce the degree of disability that a patient may experience following a stroke.
- Low complication rates: Mechanical thrombectomy is a relatively safe procedure with low complication rates.
- Time-sensitive: This treatment is a time-sensitive procedure that should be performed as quickly as possible after the onset of symptoms to maximize the chances of a successful outcome.
It is important to note that not all stroke patients are eligible for mechanical thrombectomy and that the procedure carries certain risks, so the decision to proceed with the procedure should be made on a case-by-case basis and after a thorough evaluation by a stroke specialist.
Conclusion:
The mechanical thrombectomy is a promising treatment for brain stroke that can significantly improve outcomes for patients. It is a time-sensitive procedure that should be performed as quickly as possible, and it is important that patients be assessed by a stroke specialist to determine if they are eligible for the procedure. With the help of this treatment, many stroke patients can now have a chance of better recovery and survival.
Frequently Asked Questions:
Q: What are the risks associated with mechanical thrombectomy?
A: As with any invasive procedure, there are risks associated with mechanical thrombectomy. These may include bleeding, infection, and damage to the blood vessels or surrounding tissue. However, these risks are typically low and the procedure is considered safe.
Q: How long does recovery take after mechanical thrombectomy?
A: Recovery time can vary depending on the individual and the extent of the clot. Some people may be able to return to normal activities within a few days, while others may take several weeks or more to fully recover. Your doctor will provide you with specific instructions for recovery and rehabilitation.
Q: What are the chances of recurrence of thrombosis after mechanical thrombectomy?
A: The recurrence of thrombosis after mechanical thrombectomy is rare, but it can happen. The risk of recurrence can be reduced by taking blood thinners, maintaining a healthy lifestyle, and following the advice of your doctor.
About the Author:

Name: DR . SURESH GIRAGANI
INTERVENTIONAL RADIOLOGIST
DR. SURESH GIRAGANI CONSULTANT INTERVENTIONAL RADIOLOGIST at Apollo hospitals Jubilee Hills, has more than sixteen years of clinical experience in vascular interventions with a special interest in neurovascular and peripheral vascular disease interventional procedures.